The Home Health Aide (HHA) is part of the home care team, providing personal care, and companionship to the client in their home.
The HHA will work under the direction, instruction and supervision of a Register Nurse (RN). This person will be responsible for observing patients, reporting these observations and documenting observations and care performed.

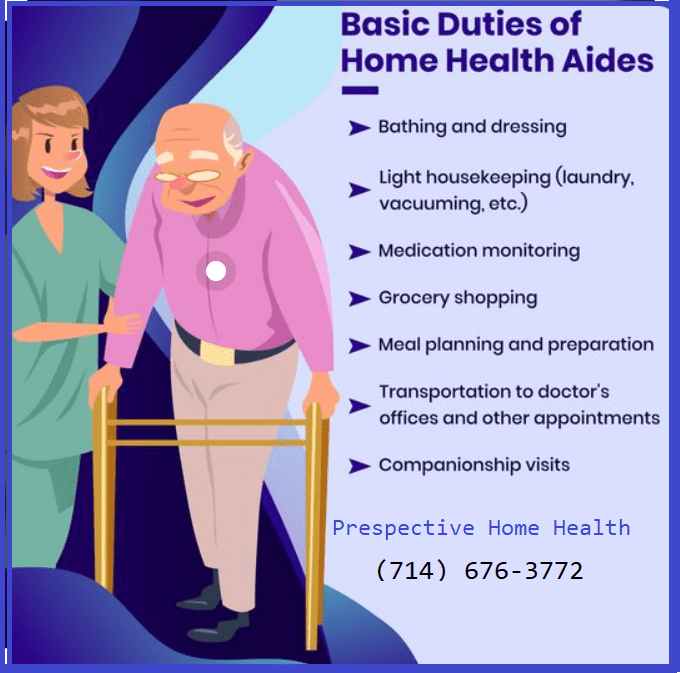
HHA Responsibilities / What Does a HHA Do?
Maintain a comfortable, safe and clean environment for patients

We will be working in the patient’s home . The patient may be in someone else’s home as well such as a daughter/son, etc. but still, a home.
This is the environment that the home care team has chosen versus an assisted living facility or a nursing home and as such it should be made as comfortable and safe as possible.
The home health aide plays a major role in this responsibility.
Examples may include picking up items on the floor, creating a safe passage to the bathroom, putting away items on the counter/stove, etc.
Provide companionship to patients

An aide may be the only person a patient sees for days and perhaps, sadly, weeks.
The HHA will listen to the patient and empathize and perhaps sympathize during these conversations. Understandably, the home aide is certainly not a social worker and no advice or guidance should be dispensed but simply listening to a patient may be the best medicine she/he needs that day.
Dress patients needs vary from minimal assistance to totally dependent

Most people take for granted pulling up their pants or buttoning a shirt.
Those who are homebound and need the assistance of a home health aide may need help with these “simple” tasks.
Our Home health Aides have learned, as part of their training, how to perform such tasks as dressing a patient whether helping them lift an arm back to put on a shirt or tie their shoes.
A HHA takes great satisfaction in helping patients and getting them dressed is one of the basic tasks performed.
Bathe patients: bed baths, tub baths or showers

A home health aide should, depending on the ability of the patient, encourage the client to bathe as often as possible.
The patient may be able to do some of this and the HHA provides the rest.
Most people will not need to bathe or shower each day though the HHA needs to make sure hands, face, and private areas are washed daily. You will need to consult the nurse on the home care team if the patient puts up a fuss about bathing.
The daily schedule created by the home care team will have the specifics along with a schedule.
Recapping some bathing skills learned at home health aide training:
Prepare: have all supplies ready before the bath
Warmth: keep the room comfortably warm
Respect: privacy should be highly respected; cover patient when possible
Suit Up: wear [latex] gloves as contact with bodily fluids and/or feces is inevitable
Toilet patients and assist with bedpans and urinals; may also help transport patients to the bathroom

A patient in the care of a home health aide may need to use a bedpan (or urinal) because she/he cannot get to the bathroom easily.
Patients should urinate regularly and have bowel movements.
Certainly, most patients will be elderly and there may be just a short warning from her/him of the urge to urinate. You need to be aware of the signs of the patient and act quickly yet calmly and help the patient.
Home health aides who see the same patients on a regular basis will develop a keen sense of when the need arises and will soon fit into a routine.
Make beds and change linens

Making/changing beds is pretty routine for home care aides and a skill set learned in training.
Many times, however, patients will not be in an actual bed but be more comfortable in a chair, couch, etc. take direction, as always, from the Registered Nurse.
Ensure that non-ambulatory patients are turned regularly, to ensure comfort and prevent bedsores

Home health aides learn in training that bedsores are much easier to prevent than to treat and much time was spent on this – hopefully!
A plan of action should be developed between the home health aide, RN and the patient – every circumstance is unique.
Changing positions is key to preventing pressure sores. In general, changes should be frequent. Proper techniques must be learned.
Provide emotional support to patients and / or family members

Home health aides help the patients with activities of daily living at home but they also provide valuable emotional support.
They are not social workers – these folks are more qualified and certified to handle complex issues.
Many times a home health aide can also be a health coach taking on additional role in the overall health of the patient. This requires a bit more training but it is a growing trend in home care.
Folks needing help at home often face emotional and spiritual distress. They need time to become adjusted to their physical limitations and they may worry about their loved ones.
If something arises from these conversations that concerns you (e.g. patient wants harm her/himself, talk of severe depression, etc.) then alert your RN immediately.
Administer medication as directed by nurse or physician

Here’s a tricky one… as it all depends.
Depends on what?
Some states have different requirements for home aides to administer medications; aides need to understand the rules and the best resource is, once again, the RN assigned to the patient’s home care team.
Usually, the home aide can help the patient “self-administer”; examples include uncapping a medicine bottle, taking a tube of cream out of the box, handing the patient her/his prescription medicine, etc.
Home health aides can remind the person when to take the prescribed medications but cannot administer them. They cannot give a tubal feeding either.
Record patient vital signs

Home health aides are on the “front line”, so-to-speak.
They are the first ones, usually, seeing the patient each day and observe changes to the overall health and well-being of the patient.
One of the ways they measure this is by taking and documenting vital signs.
Vital signs include:
Temperature (body)
Pulse (measures heart rate) rate
Respiration (rate of breathing)
Blood pressure
Accurate and detailed documentation and record-keeping are crucial.
HHA’s document these vital signs at particular times usually set by the RN. If there are significant variations in any of the vital signs then medical team needs to be notified; the HHA is not responsible for treating any changes in the vital signs.
Provide catheter care; empty and record intake / output

If the patient has a urinary drainage bag then measurements need to be taken as directed by the RN.
Measurements are to be recorded on the documentation forms provided. Urine measurements are always in cc’s (much more accurate than ounces).
This is one of the more important measures: if the patient has had more intake than output then this could be a serious condition and if the patient has had more output than intake this could be the result of dehydration.
Report all changes of a patient (physical and/or mental)

The home health aide will be responsible for notifying the nurse about any changes to a client.
These observations will be part of the “big picture” of the care the patient receives.
Example of things you will be reporting on:
observations
daily measurements
you may be ordered to record your client’s:
vital signs
weight
intake and output
blood sugar level
safety issues
client statements & complaints
unusual events
The health aide will not report these freely on a notepad: there will be forms provided by your employer on exactly what to fill out, how and when.
Questions about the form(s)? Ask the home care nurse right away!
Complete daily documentation on the care provided to each patient, accurately and completely, in the appropriate format/forms

What makes fantastic documentation on the care being provided?
Completion
Documentation should be thorough and adhere to the rules and procedures of the home health agency
Consistency
The documentation needs to be consistent if proper medical terms and abbreviations are used; adhere to the plan determined for the patient; and the RN is told immediately of changes in the condition of the patient
Legibility
If the only person who can’t read what has been documented then, really, what’s the point? The purpose of documentation is to communicate.
Accuracy Counts
Home health aides need to get it right and get it right the first time. Proper use of medical terms, correct spelling and keeping to the facts will ensure accuracy.
Timely
Proper documentation should be recorded as it happens. Waiting at the end of the shift or the next day is just not acceptable.
Home health aides are required to write down information as it happens and turn the forms in when they are due as determined by the agency. No exceptions.